Liver Disease: Types of Liver Damage
Is My Liver Healthy? Understanding Symptoms of Liver Damage
Are you noticing any unusual symptoms lately? Perhaps you’re experiencing fatigue, abdominal pain, or unexpected weight loss. While these symptoms could be attributed to various causes, they also signal underlying liver damage. Your liver plays a vital role in your body’s overall health, so it’s essential to recognize the signs that something might be amiss.
Let’s examine the symptoms associated with liver damage and how they manifest at different stages of liver disease.
Early Warning Signs
Early warning signs of liver damage may include persistent fatigue and abdominal discomfort. These symptoms are crucial indicators of potential underlying issues with liver health. Recognizing these symptoms early on can prompt timely medical evaluation and intervention to prevent further complications.
– Fatigue: Feeling unusually tired or lacking energy, even after adequate rest.
– Abdominal Discomfort: Experiencing pain, swelling, or tenderness in the abdomen, often around the liver area.
– Digestive Issues: Encountering digestive problems like nausea, vomiting, or loss of appetite.
– Jaundice: Noticing skin and eyes yellowing indicates possible liver dysfunction.

Progression of Symptoms
As liver damage progresses, symptoms may become more pronounced, signaling advancing liver disease stages:
– Dark Urine: Urine appears darker than usual due to bilirubin, a substance produced by the liver.
– Pale Stools: Stools lose their standard color and become lighter, indicating a lack of bile flow from the liver.
– Swelling: Developing swelling in the legs, ankles, or abdomen due to fluid retention, known as enema.
– Itching: Experiencing intense itching, often localized to the hands and feet, caused by the buildup of toxins in the bloodstream.
Symptoms by Stage of Liver Disease-
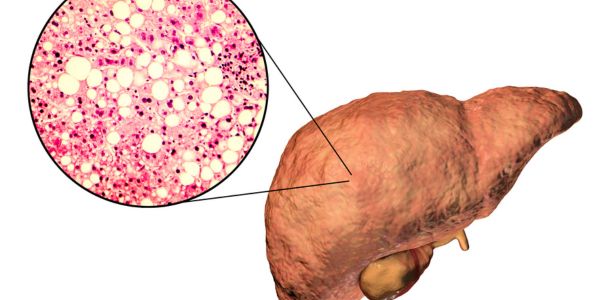
Stage 1 (Fatty Liver Disease): Fatty liver disease, often associated with Stage 1 liver damage, occurs when excess fat accumulates in the liver cells. This condition, termed hepatic steatosis, typically develops due to factors such as obesity, insulin resistance, excessive alcohol consumption, or certain medications.
In Stage 1, individuals with fatty liver disease may not experience noticeable symptoms, but they might encounter fatigue and mild abdominal discomfort. Monitoring and managing risk factors such as obesity, diabetes, and alcohol consumption are crucial in preventing progression to more severe stages of liver damage.
Stage 2 (Hepatitis): Hepatitis refers to inflammation of the liver, often caused by viral infections (hepatitis viruses), particularly hepatitis B and C. In Stage 2 liver damage, which commonly corresponds to hepatitis, symptoms such as jaundice, nausea, vomiting, and abdominal pain may emerge.
Hepatitis viruses attack liver cells, leading to inflammation, impaired liver function, and potential long-term damage if left untreated. Prompt diagnosis and management are essential in Stage 2 to prevent further progression of liver disease and mitigate potential complications associated with chronic hepatitis infection.
Stage 3 (Cirrhosis): Cirrhosis is a late-stage liver disease characterized by extensive liver tissue scarring, impairs its function. In Stage 3 liver damage, often synonymous with cirrhosis, advanced symptoms such as fluid retention, swelling (edema), and easy bruising may manifest. Cirrhosis can develop from various causes, including chronic hepatitis, excessive alcohol consumption, non-alcoholic fatty liver disease, and certain genetic conditions.
Managing underlying risk factors and complications, such as portal hypertension and liver failure, becomes crucial in Stage 3 to prevent further deterioration of liver function and improve overall prognosis.
Stage 4 (Liver Failure): Liver failure occurs when the liver loses its ability to function adequately, leading to serious health complications. In Stage 4, liver damage corresponds to liver failure, and severe symptoms like confusion, bleeding, and coma may occur, indicating a critical medical emergency.

Liver failure can result from various conditions, including advanced cirrhosis, acute liver injury, hepatitis, or certain medications or toxins. Prompt medical intervention, including possible liver transplantation, is often necessary in Stage 4 to improve survival outcomes and prevent irreversible damage to vital organs.
Diagnosis and Treatment-
Diagnosing and treating liver damage is crucial for preserving liver function and preventing further complications. Here’s an overview of the diagnostic process and treatment options:
Diagnosis
- Medical History and Physical Examination: Healthcare providers will review your medical history and conduct a physical exam to assess symptoms and signs of liver damage, such as jaundice, abdominal tenderness, and fluid retention.
- Blood Tests: Blood tests, including liver function tests (LFTs) and specific markers for liver enzymes and proteins, can help evaluate liver function and detect abnormalities indicative of liver damage or disease.
- Imaging Studies: Imaging tests such as ultrasound, CT scans, or MRI scans may be performed to visualize the liver’s structure and identify any abnormalities, such as liver enlargement, tumours, or cirrhosis.
- Liver Biopsy: In some cases, a liver biopsy may be recommended to obtain a tissue sample for microscopic examination, providing detailed information about the extent of liver damage and the underlying cause.
Treatment
- Lifestyle Modifications: Adopting a healthy lifestyle is essential for managing liver damage. This may include maintaining a balanced diet, limiting alcohol consumption, avoiding exposure to toxins, and engaging in regular exercise to promote liver health.
- Medications: Depending on the underlying cause of liver damage, medications may be prescribed to manage symptoms, reduce inflammation, or treat specific liver conditions such as viral or autoimmune hepatitis.
- Treatment for Hepatitis: Antiviral medications are available for treating viral hepatitis infections, such as hepatitis B and C. These medications can help suppress viral replication, reduce liver inflammation, and prevent disease progression.
- Management of Complications: Complications associated with advanced liver damage, such as ascites (fluid buildup in the abdomen), hepatic encephalopathy (brain dysfunction due to liver failure), or portal hypertension (high blood pressure in the liver), may require specific treatments or interventions to alleviate symptoms and improve quality of life.
- Liver Transplantation: In severe cases of liver failure or end-stage liver disease, liver transplantation may be considered a life-saving treatment option. A diseased liver is replaced with a healthy liver from a deceased or living donor during a liver transplant.
- Ongoing Monitoring and Follow-up: Regular monitoring of liver function through blood tests and imaging studies is essential for tracking disease progression, evaluating treatment effectiveness, and making necessary adjustments to the treatment plan.
Overall, early diagnosis, appropriate medical management, and lifestyle modifications are key to effectively managing liver damage and improving long-term outcomes for individuals with liver disease. Platforms like Curebridge provide access to top healthcare providers, such as hepatologists, gastroenterologists, and liver transplant specialists, ensuring tailored and comprehensive care for every patient.
Final Words
In conclusion, awareness of the symptoms associated with liver damage and disease stages is essential for maintaining overall health. If you’re experiencing any concerning symptoms, it’s crucial to consult a healthcare professional for proper evaluation and management. Remember, early detection and intervention can significantly improve outcomes and quality of life. Stay vigilant, prioritize your health, and take proactive steps to support your liver’s well-being.
People Also Read: How Does Living Liver Donation Work? 6 Things to Know
